Many GP practices do not have enough capacity for their patients’ needs. As highlighted in the GPC Wales Save Our Surgeries report, the number of patients per full time equivalent GP has increased by a third over the last decade. It is unsurprising therefore that 80% of GPs in Wales say they fear their workload is detrimental to patient care. This is causing GPs and their teams’ a great deal of stress.
The purpose of this guidance is to support GPs and their practices in difficult circumstances to safely manage their workload to a reasonable level. It can also be used as a guide by all practices to assess whether their level of service provision and patient access is consistent with the BMA’s recommendations. It is hoped that this guidance will help practices to establish a reasonable and safe workload – to protect GPs, their staff, and patients – and ultimately help maintain GP services in the long term.
This advice is specifically for GP practices operating under the Welsh General Medical Services contract and GPs working in Local Health Board Managed Practices.
Safe workload advice
Until there is better support and funding to reverse the sustainability crisis, GP practices must be prepared for increasingly difficult circumstances and further workload challenges. Many practices will need to protect themselves and their patients from unsafe consequences of excessive workload.
The GP practice workload crisis is often so serious that we recommend practices take urgent action to preserve patient care and their own wellbeing. Practices will need to care navigate and decide how to prioritise care and day-to-day activity accordingly. These actions will inevitably result in some patients waiting longer for non-urgent care, or issues that do not need to be dealt with in general practice being directed elsewhere.
GPs are reminded that Health Boards are ultimately responsible for the provision of primary medical services for patients. While LHBs contract with GP practices to deliver this responsibly, GP practices are not a safeguard for all NHS services or providers of last resort – and they cannot be expected to operate beyond the terms of their contract or undertake a workload that is unsafe.
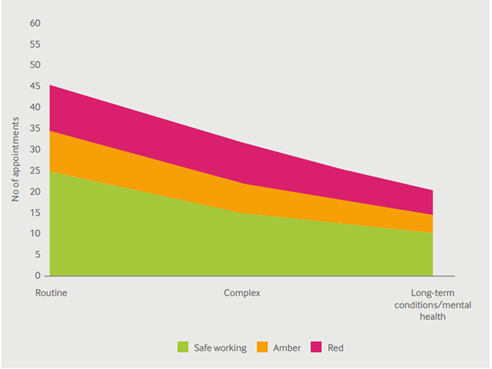
The European Union of General Practitioners and BMA have recommended a safe level of patient contacts per day in order for a GP to deliver safe care at not more than 25 contacts per day. 'At Your Service', published by the Policy Exchange and foreworded by Sajid Javid, states that 28 patient contacts per day is safe.
1. GP practices should direct patients to appropriate NHS services
GP practices can limit their workload, consistent with the advice that follows, to protect themselves, their staff, and patients.
It is acceptable for GP practices, where clinically appropriate following care navigation, to direct patients to other Health Board services including:
- The NHS Wales pharmacy Common Ailments Service,
- The Welsh Eye Care Scheme
- NHS Wales 111 for advice –including the ‘111 Press option 2’ scheme for mental health.
- For dental issues, general dental practitioners (or 111 where patients are not registered with a GDP)
- Transferring patients to OOH at the end of the working day with appropriate clinical handover.
Where these LHB services are underdelivering for patients and practices have patients returning to them, please raise with your LMC to address this with their Health Board.
Practices can direct emergency and urgent problems to other health board services including:
- GP out-of-hours at appropriate times
- Urgent Primary Care Centres (where available)
- Accident and Emergency departments,
- The Welsh Ambulance service.
2. GP practices should determine a safe level of working for all GPs in their organisation
The number of safe patient contacts reduces as complexity of the contact increases. There is evidence around decision fatigue and an increase in errors or mistakes as contact and complexity rates increase.
The decision on introducing a safe working limit protocol must be made at a practice level, with consideration of the urgency of case mix, complexity and demand. This should take into account non-patient facing clinical and administrative tasks.
We do not recommend a rigid adherence to a maximum number of contacts per day. But when developing their own protocols, we recommend that practices adopt a more flexible and forward planned approach to their capacity offer. In line with the Access Commitment within the Welsh GMS contract, this requires care navigation and prioritisation of urgent cases, with waiting lists and advance booking for non-urgent care.
3. Safe working levels should apply to duty doctors
Many practices in Wales operate with a duty doctor that picks up urgent and unscheduled care. This can be efficient - allowing other GPs to focus on planned care delivery - but also risks uncontrolled and excessive workload which is not consistent with safe working. A practice’s workload limit determination should also apply to their duty doctors.
Practices need to be aware that there is no requirement under the GMS contract for GP practices to have a duty doctor, and the BMA is increasingly concerned that duty doctors are working beyond safe levels.
Where practices choose to operate a duty doctor system, as part of their care navigation process they should include clear protocols on the type of contacts that are appropriate to be passed to a duty doctor.
Successful care navigation should ensure that duty doctors do not act as a sponge to soak up demand from patients who are finding access to the practice slower than desired.
4. GP practices should consider 15-minute appointments
The BMA strongly recommends practices take immediate measures to move to 15-minute appointments. Many practices still provide care at 10-minute or shorter intervals. This includes patient note keeping and other non-patient facing clinical tasks in between patient appointments. Without increasing the total time spent on consulting in a day, GPs can preserve quality of care, by moving to 15-minute appointments.
BMA recommends that no more than 3 hours per session is spent in consultation with patients to allow adequate time for administrative work/tasks. Within these limits, adequate rest breaks must be taken. Increasing appointment length to 15 minutes would mean a reduction in the absolute number of appointments per session to safe levels for clinician and patient.
Controlling your workload under the contract
In addition to the measures above on introducing safe levels of patient contacts, care navigating to other NHS/LHB services, and extending appointments to 15-minutes, there are several options that practices can use under the contract to help protect themselves from unmanageable workloads.
While no single option is likely to be a full solution, it may be possible through a variety of measures to reduce the workload of a practice to a level that is hopefully safe and manageable in the longer term.
We would encourage all practices to continue collecting clinical and administrative activity data alongside the contractually mandated mapping of appointment slots/sessions as recorded on the Primary Care Information Portal. This continues to strengthen the case for investment of resource into GMS and demonstrates to the public the ever-increasing workload pressure in general practice.
If your practice workload is unmanageable, you may wish to consider the following:
1. Inform the relevant Health Board and consider the Escalation processes.
Let your Health Board know that workload at your practice is regularly reaching an unmanageable/unsafe level which is impacting on your ability to provide safe care for your patients.
This can be done by completing the Escalation Framework on the Primary Care Information Portal, accessible to all practices across Wales. While the Framework applies nationally, each Health Board may have minor local variations in actions and process. Annex A provides an example in use by one Health Board.
Practices should also formally write to/email the Health Board informing them that your practice workload is unmanageable and that you are seeking the Health Board’s support to resolve the problem. Health Boards are ultimately responsible for primary care and have a responsibility to support practices.
When writing to the Health Board, communicate the reasons why the practice workload is unmanageable. Reasons may include (but are not limited to):
- Inability to meet excessive demand.
- Unfilled vacancies/inability to recruit GPs or other practice staff.
- Inadequate or unreliable HB services to patients.
- Inadequate space to accommodate the practice responsibilities.
- Insufficient financial resource, etc.
You will also want to highlight any practical help the Health Board could provide to improve the situation. Practices will want to consider the Health Board’s reply and any suggestions that might improve your workload. If the Health Board does not respond promptly or you do not consider their response helpful, you should consider implementing other aspects of this advice as deemed necessary by the practice.
You may also wish to inform your Local Medical Committee of your practice workload difficulties. LMCs are helpful in highlighting any local support or systems in place that could help your practice. In some Health Board areas, local escalation processes are in place that allow practices to reduce their services to patients if faced with serious capacity challenges.
2. GP Sustainability Assessment Framework
Any practice which considers itself vulnerable to risk of closure within 12 months and/or a reduction in the range of service provision are advised to contact their Health Board to discuss in the first instance with a view to making an application under the GP Sustainability Assessment Framework. The Local Assessment Panel will aim to make a decision within 6 weeks of receipt of the completed application for assessment.
3. Consider reviewing practice arrangements for patient access.
GP contractors are required to carry out their obligations under the contract with reasonable skill and care and to provide for their patients’ reasonable needs. Practices must exercise their professional judgement in allocating their resources in accordance with their usual ways of working. This applies to the processes the practice puts in place to allow patients to access the services they provide. Practices should regularly review their access arrangements to ensure the safe and appropriate delivery of services for patients within their practice capacity.
GP practice capacity is finite. If demand exceeds capacity, then practices should care navigate and prioritise care for those patients with the greatest need - in particular children under 16 with acute presentations and patients who have been clinically triaged to require urgent assessment.
If a practice’s safe capacity is reached on the day, following care navigation patients can be offered an appointment at a date in the future which matches the capacity of the practice, or placed on a practice waiting list. We appreciate that this would be a significant new way of work for practices and would have considerable administrative workload and possibly clinical governance aspects that the practice would need to carefully consider.
A patient’s clinical condition may well change while on a waiting list and a practice should consider reviewing the urgency at this point. Alternatively, they may consider directing the patient to another Health Board service. Practices should advise patients placed on a waiting list to call the practice again if their condition deteriorates.
4. GP practices should push back on inappropriate workload.
The All Wales Communication Standards between General Medical Practitioners and Secondary Care were published as a Welsh Health Circular in 2018. This work was informed by a report by the Academy of Medical Royal Colleges Wales and was based on the Communications Standards established by Cwm Taf University Health Board. The Welsh Government, Health Board Medical Directors and BMA Cymru Wales have endorsed the Standards. The standards remain in place and can be helpful to practices when considering workload requests from other NHS services.
Additionally, the BMA provides template letters to support GP practices in pushing back on inappropriate work from secondary care, prescribers, and health boards. Practices may use these templates to decline workload transfer where they consider that requests are inappropriate but should consider whether individual patients would suffer adversely from any dispute on responsibility. LMCs and the BMA can help practices determine if work they are being asked to do is inappropriate.
5. Managing patient complaints.
Patient complaints can be a significant source of anxiety and stress for GPs, particularly when they occur despite GPs going above and beyond to care for their patients in the face of workload challenges. Practices may worry that implementing safe working limits could lead to their practice receiving more complaints from patients who are frustrated at the level of access to appointments that the practice is able to provide.
It is important, however, to recognise that the amount of capacity that practices have available and the number of appointments they feel that they can safely offer is ultimately driven by Welsh Government’s investment and workforce planning decisions, and the level to which it wishes to prioritise General Practice. While practices have flexibility in how they deliver their services, they do not control the overall funding envelope that can be used to deliver GP services or have responsibility for ensuring sufficient new GPs are trained and existing GPs are incentivised to remain in practice. These overarching pressures are outlined in our Save Our Surgeries campaign.
Complaints about access to appointments are often complaints indirectly about government policy. While practices must treat all complaints seriously, they can and should highlight this fact to patients and may wish to suggest patients contact their Health Board concerns team, their MS or the Welsh Government to make clear that general practice needs greater resourcing to be able to provide more appointments.
Practices should also recognise that the risk of more serious complaints relating to standards of patient care falling short of what a patient expects are more likely to occur when clinicians are working beyond capacity and at increased risk of making mistakes. Implementing safe limits on workload can help reduce the chances of such mistakes occurring and serious complaints being subsequently received.
6. Consider formal practice list closure.
Practices can notify the Health Board that they wish to close their patient list to achieve a more manageable and safer workload. The minimum list closure period is 12 weeks and the maximum 1 year.
We encourage practices to engage with their LMC before pursuing a list closure application with their Health Board, as the LMC can provide detailed and valuable support throughout this process.
The process to request a list closure is documented in Schedule 3 paragraphs 38-39 of the Welsh Unified GMS Contract regulations and can be summarised as follows:
- Make the application to close the list in writing to the Health Board (HB).
- Outline in this letter to the HB what actions the practice will implement so that the list can re-open at the end of the closed period, conditional on the underlying problem being resolved (i.e., recruitment). This letter must include the period of time during which the list will be closed (minimum 12 weeks, maximum 1 year).
- The HB must acknowledge receipt of the application within 7 days.
- The HB may reasonably request further information from the practice to enable the application to be considered thoroughly.
- The HB will likely request a meeting with the practice to talk through the difficulties including considering what support they can offer and/or discuss what changes can be implemented to enable the list to remain open.
- The HB will consult with those who would be affected by the closure and should provide the practice with a summary of the views expressed.
- The HB must make a decision within 21 days, starting on the date of the receipt of the application (14 days for an extension to the closure), unless otherwise agreed with the practice – that decision is to be notified in writing to the practice as soon as possible.
Practices will want to consider the BMA’s advice above on safe working to determine a reasonable list size that would trigger the reopening of the list. Health Boards can reject applications by practices to close their list – this rejection must be conveyed in writing outlining the specific reasons why. This decision can be challenged via an appeal to Welsh Ministers via the NHS dispute resolution procedures.
It is important to note that where a Health Board wants to assign patients to a closed practice list, they must prepare a proposal for consideration by an assessment panel (which must include LMC representation) prior to doing so. This is described at Paragraph 45 of the regulations. Should a practice wish to dispute this decision, an appeal can be made to the Welsh Ministers.
7. Consider reducing provision of supplementary services to maintain core services.
Practices are not obligated under the 2023 Unified GMS contract to provide supplementary services (local, national, or directed). Practices can serve notice to the Health Board if they wish to cease supplementary services. This will impact practice funding but may enable practices to deliver core services better or ultimately stop delivering services at a loss. Practices should consider whether it is cost effective to continue providing supplementary services and how any such decision will affect their sustainability.
Through negotiations with Welsh Government, GPC Wales has progressively moved historical funding and the work attached from ‘non-core’ elements like clinical QIF into the global sum. Under the new unified contract, practices can no longer opt out of providing additional services, but the associated funding has consolidated into global sum.
Principles of maintaining practice profitability
This document is designed to outline practical steps that you can take within your own practice to consider how you can stem rising costs.
The two main principles of maintaining profit are:
- maintaining revenue as a minimum/increasing revenue
- controlling expenditure/reducing cost
Conclusion
General practice in Wales is under intense and increasing pressure. Difficult decisions need to be taken by commissioners of care to invest in GMS before it is too late, and more practices become non-viable. It is inevitable that the capacity gap created by years of underinvestment in GMS will mean patients having to wait longer for routine care, even as demand rises inexorably. Protecting the quality of care, you deliver and the workforce that delivers it should be paramount in this environment.
Practice teams need to consider the contents of this document carefully and implement those measures they feel are necessary to protect the quality of care they offer and the wellbeing of their workforce.
Care navigation of requests is central to controlling your workload – it is contractually required under the access commitment and vital to ensuring the right cases are dealt with at the right time in the right place.
In the current climate it is vital you ensure you work to your contract and consider those elements outside what is contractual carefully in the round. Whatever you choose to do, ensure the whole practice team, and your patients, are aware of any changes you implement. If you have any issues, contact your LMC and the BMA for support.