The impact on doctors’ health from moral distress and moral injury can be significant, being linked to severe mental health conditions such as depression and PTSD.
This is a result of the institutional and resource constraints healthcare staff face, meaning they often cannot provide the high level of care they want and expect to be able to deliver.
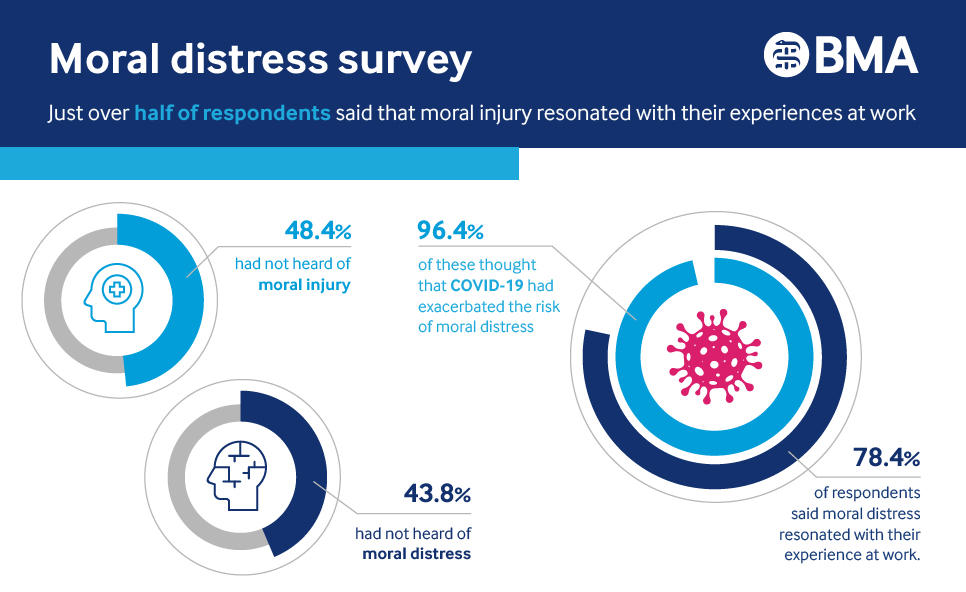
From March to April 2021, the BMA surveyed all doctors throughout the UK on the issues of moral distress and moral injury. More than 1,900 doctors responded.
This report is based on the findings of the BMA’s review of this problem in the NHS. This included interviews and discussions with doctors, analysis of academic research, and the survey.
You can download the full version of this report below.
 Survey stats
Survey stats
What is moral distress?
Moral distress is where institutional and resource constraints create a sense of unease among doctors from being conflicted about the quality of care they can give.
At a time where resources are stretched, doctors cannot provide the quality of care they want to, and this has a negative impact on them as well as patients.
- 43.8% of survey respondents had not heard of moral distress.
- 48.4% had not heard of moral injury.
When learning more about the definitions:
- 78.4% said that moral distress resonated with their experience at work.
- 51.1% said that moral injury resonated with their experience at work.
Moral distress refers to the psychological unease where professionals identify an ethically correct action to take but are constrained in their ability to take that action.
Even without an understanding of the morally correct action, moral distress can arise from the sense of a moral transgression.
More simply, it is the feeling of unease from situations where institutionally required behaviour does not align with moral principles.
This can be as a result of a lack of power or agency, or structural limitations, such as insufficient staff, resources, training or time.
The individual suffering from moral distress need not be the one who has acted or failed to act; moral distress can be caused by witnessing moral transgressions by others.
Moral injury can arise where sustained moral distress leads to impaired function or longer-term psychological harm.
Moral injury can produce profound guilt and shame, and in some cases also a sense of betrayal, anger and profound 'moral disorientation'. It has also been linked to severe mental health issues.
The nature of a doctor’s job often requires extremely serious decisions about a patient’s health and wellbeing. Physicians do not operate in systems with infinite time, resources and trained professionals. Difficult choices do have to be made, sometimes life-and-death decisions. These are an acknowledged aspect of medical practice.
What should not be are decisions made while under institutional limitations that violate professional standards.
The causes of moral distress in medical staff are varied but they are often consistent across countries. Doctors can experience moral distress due to:
- lack of agency to make the best decisions for patients
- insufficient resources or non-existent resources to provide care to suitable professional standards
- practical experience of medical care clashing with ethical standards taught at medical school
- being involved in wrongdoing
- end-of-life care decisions.
Repeatedly experiencing this can increase the likelihood of moral distress.
I hadn't heard of moral distress or injury before but they really explain how I've been feeling since I started work as a doctor. We are taught such high ideals to work towards as medical students and told we have the power to make changes. However the reality of working in the NHS is very different and I did become depressed when I struggled to live up to these ideals.Survey respondent
Moral distress in the NHS
There is an increasing belief across the UK that the problem of moral distress is getting worse, and this began before the pandemic.
Years of underfunding, increasing layers of bureaucracy and less autonomy for doctors contribute to a number of problems.
Many UK doctors report being forced to make suboptimal decisions for patients based on institutional constraints, leading to moral distress.
Some report the system they work in tends to imply the failing is with the doctor and that they lack resilience.
Research suggests there is a rising prevalence of moral injury in healthcare workers across many nations.
For example, there is evidence linking the significant technological investment in the US healthcare system to reduced autonomy for medical professionals, contributing to moral injury in doctors.
Top causes of moral distress in the NHS
Many of the recognised direct causes of moral distress in doctors (such as seeing poor quality of care and end-of-life decisions) were explained above. The factors respondents were asked about mainly referred to structural deficiencies that contribute to moral distress.
The graph below shows the top 15 answers to a question from the survey asking respondents to list the five most important causes of moral distress in their opinion.
| Reason | % of votes |
|---|---|
| Not enough staff to suitably treat all patients | 52.5% |
| Individual's mental fatigue | 40.8% |
| Lack of time to give enough emotional support | 37.2% |
| Not able to give timely treatment | 37.2% |
| Deprioritising certain patients | 36.3% |
| Denying the families of dying patients access to see them | 35.9% |
| A culture that does not encourage speaking up | 28.7% |
| Guilt over risk of infecting friends and family with COVID-19 | 28.1% |
| Lack of agency to make correct decisions for patients | 25.2% |
| Lack of beds | 22.8% |
| Lack of PPE | 22.5% |
| Physical fatigue | 21.6% |
| Public health decision affecting populations | 19.5% |
| Putting your own/colleagues' safety before the patient's | 17.2% |
Moral distress and COVID-19
Many doctors have found themselves working under extraordinary, constantly evolving conditions during the pandemic, thrust into situations which do not complement their expertise and often with inadequate equipment and protection.
Doctors have said that in some specialties, there has been a loss of team building and sense of isolation that the pandemic has produced. This has meant many have felt 'alone' when making difficult decisions.
Added to this, phone consultations and referring those who have serious conditions to ever-growing waiting lists contribute to discomfort.
It is little wonder that the risk of moral distress has increased for many doctors during the pandemic.
Out of the respondents who had experienced moral distress:
- 86.2% had experienced moral distress in relation to their ability to provide care during the pandemic.
- 70.8% had experienced moral distress in relation to a colleague's ability to provide care.
- 96.6% of those who just saw COVID patients had experienced moral distress.
While COVID-19 may have aggravated the issue of moral distress for many in the NHS, it did not create it. The issue existed before and undoubtedly will exist after.
Though 83% of respondents thought it was much more likely and over 96% thought it was more likely to some extent due to the pandemic, 60% acknowledged experiencing moral distress prior to COVID-19.
Interestingly, a number of emergency medicine doctors who responded to the survey said that moral distress had been worse for them prior to the pandemic.
Several thought this was related to fewer people vising A&E due to lockdown and that the winter crises in the NHS had been worse for moral distress than the pandemic.
The pandemic has shone a light on the issue and perhaps given the push to take action.
Moral distress and injury were with us before COVID-19. They were institutionalised into the NHS system and nothing was done about them. The pandemic has focused attention on them as it is visible to all.Survey respondent
Inequalities
The survey indicated there were contrasts in results between different groups of doctors.
- 58.9% of respondents who said they have a long-term disability or physical or mental health condition said that moral injury was consistent with their experiences, compared with 48.4% of those without a disability.
- 82.6% of respondents under 55 said that moral distress was consistent with their experiences, compared with 67.7% of those above 55.
- 88.4% of doctors from ethnic minority backgrounds said that moral distress was consistent with their experiences at work, compared with 75.6% of white doctors.
- 84.5% of resident doctors said that moral distress was consistent with their experiences at work compared to 78.3% of consultants and 75.3% of GPs.
We also look at further themes in the full report, such as the breakdown of groups of doctors and what they consider to be the biggest factors causing moral distress and the impact of COVID.

We have a range of services to support you.
- Counselling
- Peer support
- UK wellbeing support directory
Call our free and confidential helpline on 0330 123 1245
What can be done?
I have found when I had opportunities to talk to senior management, they have been patronising and publicly dismissed my thoughts in front of our colleagues. I find their lack of interest or engagement with frontline colleagues hugely distressing.Survey respondent
Steps that need to be taken structurally
It is clear from our survey that many of the causes of moral distress in the UK medical workforce stem from not enough resource, such as lack of beds or time.
Substantially increased levels of investment in our health system will help ensure doctors are satisfied with the level of care they provide their patients.
Many doctors believe the reason that they struggle is because there simply are not enough doctors and other healthcare staff to meet patient demand.
The problem is likely to get worse, as this survey (and others from the BMA) indicate more doctors are intending to reduce hours and/or retire early.
The number of vacancies in the NHS have become notorious. We continue to raise recruitment and retention with government and lobby on safe staffing.
The term moral distress originated in nursing due to their perceived lack of agency.
Doctors experience the same due to the perception that decisions on patient care are being taken out of their hands and into those who may not necessarily have clinical expertise, including non-clinical managers. This is a common cause of frustration among doctors.
Medical professionals need to feel like they can raise issues without fear of reprisal. They can then voice concerns and challenge problematic systems. This also provides a more supportive workplace.
Many respondents to our survey stated a change of workplace, with a different culture, greatly reduced their exposure to moral distress.
This should be applied to all staff working in NHS trusts or equivalent organisations. You can see further work the BMA has done in this area.
In the UK, all employers have a duty of care to their employees. That can include a duty to provide aftercare support to employees who have been through emotionally stressful experiences. This includes, for example, specialist occupational health services
It is important that clear lines of emotional and psychological support are provided to healthcare workers. Staff should be encouraged to seek and be signposted to support at an early stage.
The BMA has produced a number of pieces of guidance on staff wellbeing. For example, we recently developed a wellbeing checklist which includes simple measures that organisations can implement to improve doctors' wellbeing.
A common complaint is that the NHS bureaucracy is overly complex, which can delay patient care, and make the reasoning for some patient decisions unclear. Streamlining this system could help resolve this.
Steps that you can take to empower yourself
As BMA research shows, many doctors are unfamiliar with the terms, but find it a great relief when the concepts are explained to them.
It helps people to know that their feelings are not unique and are (unfortunately) common throughout the workforce. This can help lessen the burden the individual feels.
We cannot address problems that we do not acknowledge exist. By talking about moral distress and moral injury, we recognise these issues and can look to tackle them. This becomes easier as the concepts become more mainstream.
It is important for people to able to reach out when they’re struggling without fear of judgement and to know colleagues support them.
Schwartz rounds, CPD groups, doctors’ messes, groups led by a trained facilitator such as balint groups or more informal spaces can all be helpful to do this.
It is essential that doctors are given the time to participate in such activities.
If you are uncomfortable with decisions or resourcing, it can help both the situation and the individual to speak out on this.
This can not only encourage others to do the same, but build a more healthy working culture where doctors feel empowered to discuss decisions that they think are not optimal for patient care.
The BMA recognises, though, that this is not always possible. 28.7% of respondents who had experienced moral distress stated that 'a workplace culture that does not encourage 'speaking up'' is one of the top five causes of moral distress.
It is on the organisations to build these cultures before individuals can take steps themselves, which is why the structural recommendations take precedent in this report.
Sometimes, when taking a decision, it can be reassuring to check-in with an expert or colleague on your thought process if possible.
In some instances, local ethics committees have been created which doctors can find useful when facing a tough choice. The BMA is always happy to help with any queries.
Although it may seem obvious, it is important for medical professionals to take the time to look after themselves.
Physical and mental fatigue both contribute to moral distress and injury, potentially worsening their effects. Finding the time for nutrition, exercise and rest can all help. The BMA’s wellbeing services are available 24/7. You do not have to be a BMA member to use many of our wellbeing services.

We're here to stand up for your rights, support you in the workplace and champion the medical profession.