Over the past decade social care has undergone significant reform in terms of the strategic approach to adult social care, the structure and how services are delivered.
An important theme has been a move towards greater integration between health and social care, as seen with the creation of IJBs (integrated joint boards).
Another distinguishing characteristic of the Scottish system is the entitlement to free personal care for those aged 65 years and over.
Who receives social care?
- In January 2016, 61,500 people received home care in Scotland and 36,000 adults were in care homes.
- Data from 2010/11 shows that 90% of people over 65 years who received personal care from a local authority were not charged for these services.
- A significant proportion of adult social care provision delivered by informal unpaid carers.
- The Scottish Government has estimated that there are around 788,000 unpaid carers in Scotland. This includes 44,000 people under the age of 18.
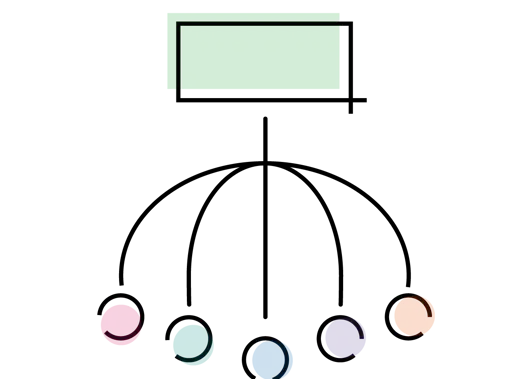
How social care is structured
The Scottish Government sets out the overall strategic framework and legislative basis for the delivery of adult social care. It decides outcomes which local authorities are expected to achieve.
Local authorities have a statutory responsibility to provide adult social care services. To deliver an integrated service, local authorities and NHS boards work together.
In the majority of cases this is achieved through an IJB. IJBs are responsible for the planning of adult social care services, as well as some health services and other functions.
Paying for social care
- Unlike healthcare, some elements of adult social care in Scotland are chargeable.
- A distinguishing characteristic of the Scottish system is, however, that there is an entitlement for free personal care for those aged 65 years and over.
- Payments for personal care are universal and are not means tested.
- Local authorities have flexibility in the interpretation and implementation of the free personal care guideline.
- In 2010/11 the cost of home care for those aged 65 and above was £406.7 million, 37.7% of which was spent on personal care services.
- For people aged 65 years and over charges for the personal care component of residential care are covered by personal care payments.
- Accommodation charges take into account user's capital, which includes savings and property, above which users pay the standard rate for care - £25,250.
- For capital between £15,500 and £25,250 the individual’s contribution will be calculated depending on their capital.
- Under this amount, users will not be required to make any contribution towards their care from capital but will be required to contribute from their eligible income.
Pressures on social care
Social care, like healthcare, is facing unprecedented pressures. These pressures are coming from increasing demand, alongside funding and workforce constraints.
Increasing demand
- The population is expected to grow 7% by 2039.
- At the same time the number of people aged 75 years and over is projected to increase by 85%.
- A greater number of people are living with multiple long-term conditions. As a result a greater combination of different social care services are needed.
Funding constraints
- Since 2010/11 local authority total revenue funding has reduced by 11% in real terms, while social care spending has increased by 3%.
- If local authorities and IJBs continue to provide services in the same way, social care spending will need to increase by between £510 and £667 million by 2020 (16-21%).
Workforce challenges
There are huge challenges with recruiting and retaining social care professionals.
In addition migrant workers make up a large proportion of the adult social care workforce. As a result of the UK leaving the EU, there are now uncertainties in the future of EU care workers’ status in the UK.
The BMA's view
Social care is an increasing area of concern for the BMA.
We believe that significant pressures in social care are a direct result of inadequate resourcing. To look after patients well, doctors need social care to be well-funded and adequately staffed.
Effective engagement of doctors, particularly GPs, will be key to the success of the integration agenda.