The NHS is the fifth largest employer in the world, with 47% of NHS staff now aged 45 or over. Six out of 10 consultants and SAS doctors are over the age of 45 and nearly one in every two GPs are over the age of 45.
Many doctors are finding working in today's NHS too taxing on their work-life balance, particularly as they age, causing some to seek early retirement.
Key findings of the report
- Early retirement in the medical workforce leads to a loss of expertise and skills in an already understaffed workforce.
- Older doctors act as role models, supervisors and appraisers.
- Older patients place unique value in being treated by an older doctor, which can strengthen the relationship between patient and doctor.
- Understanding the reasons doctors are retiring early is important so that the NHS can work out what will motivate them to stay and how they can be supported.
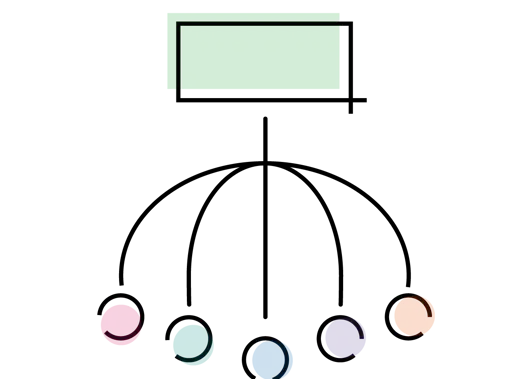
BMA recommendations for employers
Make it easier for an older workforce to work in the NHS so their skills and experience can be retained
- Trusts/health boards and practices should support, develop and promote part-time or flexible working for staff across their medical careers.
- Prior to advertising a post, employers should consider whether it can be filled by someone who wishes to work part-time or whether they would consider someone who wanted to work flexibly.
- Employers should schedule 'transition to retirement discussions' with their staff to understand what support they might need to help them remain at work, should they wish to do so.
- To ensure they are healthy, fit and able to work, senior doctors, alongside other NHS staff, should have access to a free specialist-led occupational health service.
- Employers must support their older doctors by ensuring they are getting enough rest breaks and have appropriate facilities when staff are suffering from fatigue.
Make it easier for older doctors to contribute their skills in other ways
- Are other non-clinical opportunities available, such as working in management, teaching research or as appraisers.
- Many opportunities to work in local health service development or teaching require current engagement in clinical work. This barrier must be re-assessed so that doctors who are retired from clinical practice are able to take part in this work.
- It is currently possible for retired doctors to act as appraisers, however appraisers should have a licence to practice and ideally still be in clinical practice - this should be for no more than three years post-retirement.
Ensure doctors are not disadvantaged financially by coming back from retirement
The Government should undertake a full review of the pensions tax relief systems, including the impact of annual allowance on workforce planning and pension scheme membership.
Survey results
Following a survey of a small sample of doctors of all grades working in different settings in the UK, we found that:
- when considering retirement, health and wellbeing (85%) was the most important factor followed by workload (66%) and burnout (61%)
- in actually making the decision to retire, job satisfaction (60%) and working patterns (57%) also play a significant role
- the most important factors that would influence a decision to work past the retirement age are the ability to work flexibly (65%), job satisfaction (57%), having time to practice the most enjoyable aspects of medicine (50%) and support with workload (44%)
- providing flexible working arrangements (25%) was the most important way in which employers could support older doctors who are still in the workforce.