Junior doctors and consultants taking joint industrial action for the first time in NHS history say they feel a greater sense of camaraderie through their combined efforts to fight for fair pay and conditions.
The 24 hours of co-ordinated action in England began at 7am Tuesday (September 20), with joint action overlapping between two days of consultant strikes and a three-day junior doctors walk out.
Both groups of doctors have seen their pay erode substantially and are calling for it to be restored to 2008 levels.
Each group has had a sub-inflation pay uplift imposed on them by the government this year, with prime minister Rishi Sunak saying the six per cent for consultants and six per cent plus a lump sum for junior doctors is ‘final’.
Simon Walsh, an emergency medicine consultant picketing outside The Royal London, said: ‘We are all here regrettably because the situation has now gotten to the point where government isn’t even willing to talk to us, let alone produce a credible offer.
‘Despite supporting each other, none of us want to be on strike. We’d all rather be at work.’
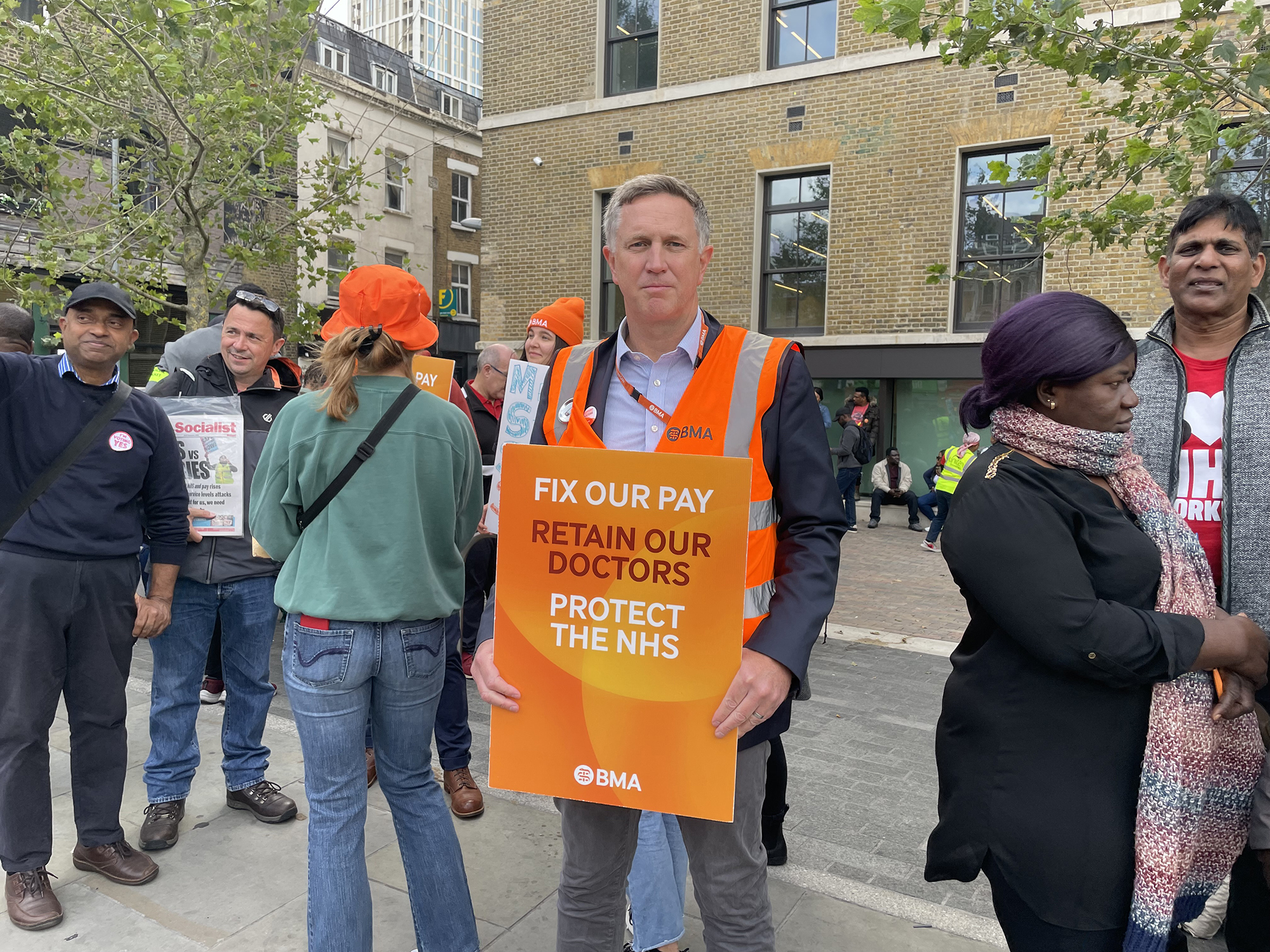 WALSH: Would prefer to work
WALSH: Would prefer to work
Dr Walsh, deputy chair of the BMA’s consultants committee, added: ‘If the government hadn’t entrenched themselves in a ludicrous position where they won’t talk to us, perhaps we wouldn’t be here.’
Margarita Kousteni, an ST2 in psychiatry at Maudsley Hospital in south London, said: ‘It’s encouraging that doctors who have gone through what we’ve gone through and reached the grades we’re aspiring to, are supporting us.
‘They know the hardship we go through and have seen better days in the NHS so can recognise things are getting worse.’
Mike Andrews, an IMT3 at Royal London, said the lack of government interaction with negotiations meant doctors and consultants are ‘hunkering down’ for a long-term dispute.
He said the recent reballot of junior doctors, in which 98 per cent voted in favour of extending the strike mandate, from a turnout of 71 per cent, shows the government’s position has ‘far from dissuaded us', adding: ‘More and more people are engaged.’
 ANDREWS: 'Hunkering' down
ANDREWS: 'Hunkering' down
The public backs doctors calls for the government to come to the table, with 70 per cent of respondents to a survey released this morning agreeing it is important or very important that government re-opens talks with doctors on pay.
It has been more than 170 days since health secretary Steve Barclay spoke with the BMA’s junior doctors committee and while consultants hailed a ‘significant step’ of fresh talks with government over the weekend no agreement has been reached. At the time of the survey, it had been a similar length of time since Barclay had spoken to the BMA’s consultants committee.
Dr Walsh said: ‘We’ve been desperate to get round the table, endlessly saying how important it is.
‘We can see that patients understand that the only way to resolve this dispute is through negotiations and listening to each other. Other NHS organisations are saying the same. It’s only the government that doesn’t want to get round the table.’
Solidarity abound
Shane Delamont, a neurology consultant picketing at Kings College Hospital, said joint strike action had brought junior doctors and consultants closer together.
‘We’ve certainly gelled much more than before,’ he said. ‘Which is a good thing, paradoxically.’
He said NHS funding pressures since the David Cameron-led government’s first austerity policies had laid the ground for the current industrial action, with doctors losing even more patience with the government’s continued lack of support after their enormous efforts during the COVID pandemic.
‘I never thought, as a consultant, I would go on strike,’ added Dr Delamont. ‘It’s built up over a number of years. What we are seeing now is the chickens coming home to roost. The anger is unsurprising.’
Phil Kelly, a consultant physician at Kings, said: ‘It’s very sad that we’ve gotten to this position where two parts of our union feel like we have to do this. At the start, some felt this might be inevitable, but it’s still sad now we’re here. That it has come to this is distressing.
 KELLY: Doctors are undervalued
KELLY: Doctors are undervalued
‘If someone had have said 15 years ago that it would get to this from where we were, we wouldn’t have thought it was possible. This is a dreadful situation, incredibly sad. We all depend on each other to do our jobs, and we are losing brilliant people.’
While the dispute is centred on pay, Dr Kelly said that, for consultants, this boiled down to a ‘currency of recognition’.
‘We are undervalued,’ he said, noting how more consultants are retiring sooner, moving overseas, going private or leaving the profession in increasingly numbers.
Dr Kelly said many consultants regularly work extra hours to fill gaps left by the workforce crisis, and that this can misconstrue average salaries as well as causing stress and burnout.
‘The average contribution is far greater than the pay’, he added. ‘And the more you say to people that they are worth less, the less they are going to be available.’
He stressed the importance of the Review Body on Doctors' and Dentists' Remuneration (DDRB) being truly independent in consultants’ negotiations with government – one of BMA consultants’ key asks.
‘The trust has gone,’ he said of the body that a Tory backbencher recently told the i newspaper produced recommendations that are ‘basically rigged’.
Government reaction
Tuesday’s joint action came after health secretary Steve Barclay announced a consultation on minimum staffing levels in hospitals during strike action.
In reaction, Phil Banfield, chair of BMA council, said: ‘If this government was serious about patient safety, it would not have deliberately run down the health service over the last 10 years, with the terrible, adverse effects that austerity has had on the health of the nation every day.’
Doctors on picket lines agreed.
Dr Kousteni said: ‘It’s up to the government to introduce the pay conditions that will make the workforce safe again.
‘Doctors need to have the incentive to stay in the NHS and be happy to work there.’
Dr Kelly added: 'To suggest minimum service levels now is sadly political manoeuvring that smacks of designing a way to break the ability to strike. If the role is so critical, pay fairly for it.’
 KOUSTENI: Doctors need an incentive
KOUSTENI: Doctors need an incentive
Dr Andrews said: ‘If the government really cared about minimum staffing levels, then they should be negotiating with us so we can get back to work and have safe staffing on non-strike days.’
Marta Patyjewicz, an FY3 at Royal London, moved from Poland to the UK expecting to have a better work-life balance in the NHS but has found herself on strike within months.
While ‘both systems are similar’, she says the NHS is ‘more overwhelming’ for doctors because of the problems caused by the workforce crisis.
Dr Patyjewicz said many fellow international medical graduates (IMGs), who are often filling gaps left by UK-trained doctors moving overseas, are moving again after a short period because of the conditions they find – which was affecting the NHS’ reputation worldwide as well as failing to resolve staffing shortages.
‘I live in London and have met lots of people in other professions, like finance, who earn a lot more than doctors,’ she added. ‘It makes you feel unappreciated.’
Naresh Buttan, a consultant psychiatrist at Maudsley, moved to the UK from Australia in 2008. In that time consultant pay has eroded by over a third in real terms.
‘Since I moved here I’ve only known pay getting worse,’ he said. ‘At the same time working conditions have become harder and harder.
‘The number of referrals has gone up, conditions are more and more complex and we have been through COVID. I’m 54 and I wonder if I can do another 10 years in the NHS. I’d love to but the way it’s going the more I think about quitting.
‘It used to be that working for the NHS you knew it would look after you, but now it doesn’t feel the same way – which is why these strikes are happening today.’
 PATYJEWICZ: NHS reputation at risk
PATYJEWICZ: NHS reputation at risk

